Sleep apnea is a serious condition affecting health in multiple ways. CPAP therapy is the primary treatment, but recent research suggests alternative therapies such as oral appliances and nerve stimulation. Understanding and managing sleep apnea can significantly improve quality of life.
What is Sleep Apnea?
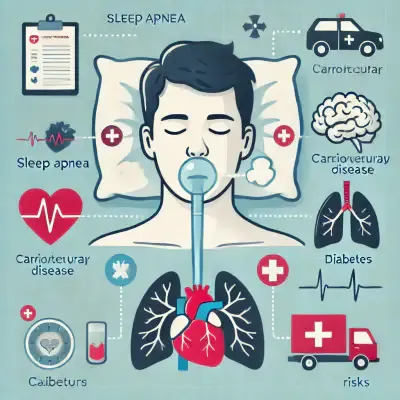
Sleep apnea is a sleep disorder where breathing repeatedly stops or becomes shallow during sleep, leading to decreased oxygen supply to the body and poor sleep quality. This condition is associated with severe health issues, including cardiovascular diseases, diabetes, and strokes.
Types of Sleep Apnea
Obstructive Sleep Apnea (OSA): The most common type, occurring when the airway becomes partially or completely blocked.
Central Sleep Apnea (CSA): Caused by the brain failing to send proper signals to control breathing, often linked to neurological disorders.
Mixed Sleep Apnea (MSA): A combination of OSA and CSA, frequently emerging after CPAP therapy begins.
The Rising Prevalence and Risk Factors of Sleep Apnea
The number of sleep apnea patients has surged in recent years, reflecting a global trend. Studies show that sleep apnea prevalence has increased worldwide, with an estimated 936 million adults affected globally, according to a 2019 study published in The Lancet Respiratory Medicine. According to the Health Insurance Review & Assessment Service of South Korea, cases rose from 45,067 in 2018 to over 153,802 in 2023.
Key Risk Factors
Obesity: Increased fat deposits around the airway can lead to obstruction.
Aging: Muscle tone loss in the airway with age can cause it to collapse.
Structural Factors: Enlarged tonsils, a small jaw, or a deviated nasal septum can contribute to the condition.
Smoking & Alcohol Consumption: Both relax airway muscles, worsening sleep apnea.
Diagnosis Methods for Sleep Apnea
The primary diagnostic method is Polysomnography (PSG), a sleep study conducted in a clinical setting. Home sleep apnea tests using wearable devices can also aid in initial diagnosis.
Sleep Apnea Diagnostic Criteria
Apnea: Breathing stops for 10 seconds or longer.
Hypopnea: Reduction in airflow by at least 30%, coupled with a 3-4% drop in oxygen saturation.
Apnea-Hypopnea Index (AHI):
Mild: AHI 5-15 episodes per hour
Moderate: AHI 15-30 episodes per hour
Severe: AHI 30+ episodes per hour
Accuracy of Home Sleep Tests
Recent studies show that home sleep apnea devices correlate well with clinical PSG but may be less accurate. Wearable devices can misread oxygen saturation due to movement and fail to detect apnea severity. A 2022 study published in the Journal of Clinical Sleep Medicine found that home sleep apnea tests had a sensitivity of 83% but a specificity of only 65% when compared to polysomnography, indicating a higher likelihood of false positives or negatives in certain cases. Therefore, clinical sleep studies remain the gold standard for precise diagnosis.
Health Impacts of Sleep Apnea
Cognitive Decline & Dementia Risk
Oxygen deprivation during sleep can lead to brain cell damage, increasing the likelihood of Alzheimer’s and other neurodegenerative diseases.
Studies indicate that individuals with sleep apnea are 1.8 times more likely to experience cognitive decline, with older adults being particularly vulnerable due to age-related cognitive decline already being a risk factor.
Cardiovascular Risks
Sleep apnea significantly raises the risk of hypertension, heart attacks, and strokes.
Many patients experiencing Wake-Up Stroke (a stroke occurring upon waking) have underlying sleep apnea.
Diabetes & Metabolic Syndrome
Sleep apnea is linked to increased insulin resistance, heightening the risk of diabetes.
The Endocrine Society reports that over 50% of sleep apnea patients also suffer from diabetes.
Standard Treatment: CPAP Therapy
Benefits of CPAP Therapy
Significantly improves sleep quality.
Clinical studies show that patients who use CPAP for three months exhibit better cognitive function and stable blood pressure.
Challenges in CPAP Compliance
Surveys indicate that only 26% of sleep apnea patients are aware of CPAP therapy.
Long-term adherence remains an issue:
75% continue treatment after one year.
Only 50% continue after two years.
The most common reasons for discontinuation include discomfort with the CPAP mask, dry mouth, nasal congestion, and difficulty adapting to the airflow pressure.
Solutions such as personalized mask fittings, heated humidifiers, and gradual acclimatization programs have been shown to improve compliance rates.
Latest Research & Alternative Treatments
Behavioral Therapy
Lifestyle changes can help mitigate sleep apnea symptoms.
Regular Exercise: Aids weight loss, which improves airway stability.
Sleeping Position Adjustments: Side-sleeping can prevent airway collapse.
Reducing Alcohol & Smoking: Alcohol relaxes airway muscles, and smoking increases airway inflammation.
Device-Based Therapies
CPAP (Continuous Positive Airway Pressure): The gold standard for OSA treatment.
Oral Appliances (OA): Mandibular advancement devices that reposition the lower jaw to keep airways open, suitable for mild to moderate cases.
Surgical Treatments
Surgery is an option when other treatments fail or when anatomical factors play a role.
Nasal Surgery: Helps correct deviated septums, nasal polyps, or chronic sinusitis.
Pharyngeal Surgery: Procedures like Uvulopalatopharyngoplasty (UPPP) widen the airway.
Jaw Advancement Surgery: For patients with small or recessed jaws, moving the jaw forward can improve airflow.
A 2023 study by the American Academy of Sleep Medicine (AASM) highlights Hypoglossal Nerve Stimulation (HGNS) as an effective alternative for CPAP-intolerant patients. Additionally, clinical trials indicate that 50% of moderate OSA patients show improvement with oral appliances.
Key Alternative Treatments
Oral Appliance Therapy (OAT):
Moves the lower jaw forward to maintain airway patency.
Recommended for mild to moderate sleep apnea patients.
Hypoglossal Nerve Stimulation (HGNS):
Stimulates tongue muscles to prevent airway collapse.
Effective for severe OSA patients who struggle with CPAP use.
Lifestyle Modifications:
Weight loss, smoking cessation, and positional therapy can alleviate symptoms.
Studies show that losing 10% of body weight can reduce sleep apnea severity by over 30%, particularly in overweight and obese individuals, as excess fat deposits around the airway contribute to obstruction.
Conclusion
Sleep apnea is more than just a sleep disorder—it is a serious health condition that can lead to life-threatening complications. Timely diagnosis and treatment are crucial. While CPAP therapy remains the primary treatment, oral appliances, nerve stimulation, and lifestyle modifications provide viable alternatives. Choosing the right therapy based on individual needs is essential.